White Paper: Medical Marijuana
White Paper on
MEDICAL MARIJUANA
Table of Contents:
I. Marijuana Use in Tennessee
II. Marijuana and Addiction
III. Marijuana and Education
IV. Marijuana Use and Safety
V. Marijuana and the Social Economy
VI. Marijuana Use and Medical Ethics
VII. Glossary
VIII. References
Marijuana Use in Tennessee
Current marijuana use among adolescents in Tennessee is reported by the Centers for Disease Control and Prevention (CDC) to be 21.4 percent, which is lower than the national rate of 23.4 percent1. States with medical marijuana laws are positively associated with increased marijuana use as access and availability to the substance increases with legalization2. Historical research has demonstrated that illegal drug use among youth increases as perception of risk and social disapproval declines; however, national perception of harm for regular marijuana use has declined sharply since 2008, when 52 percent of high school seniors believed using marijuana regularly was dangerous, compared to only 39.5 percent in 2013. The rate of adolescents in Tennessee using marijuana in the past 30 days (21.4 percent) has surpassed those who report smoking cigarettes (15.4 percent) and has increased since 2011 (from 20.6 percent in 2011 to 21.4 percent past 30 day use in 2013). Meanwhile, national trends for past 30 day use of alcohol (33.6 percent in 2011 to 28.4 percent in 2013) and tobacco (21.6 percent in 2011 to 15.4 percent in 2013) have declined. 1
Marijuana and Addiction
One in 11 people who ever start using marijuana become addicted.9Initiation of use during adolescence increases the addiction rate to one in six.17Furthermore, for those who have used the drug at least one time, the risk of becoming addicted is roughly nine percent. Of those who begin using during adolescence, the risk of becoming addicted is 17 percent: for those who get high daily, the risk is 25 to 50 percent.11 More than two-thirds of treatment admissions across the country involving those under the age of 18 cite marijuana as their primary substance of abuse, more than 15 times the rate for alcohol alone.5
Age of initiation is critical as children who smoke marijuana for the first time under the age of 14 are more than five times as likely to abuse drugs as adults.11 To compound the issue, marijuana potency has nearly tripled in the past 20 years. Currently, the average level of THC in seized samples of marijuana is 15.1 percent, compared to an average of less than 4 percent in 1983.3Concentrated forms of marijuana used in vaporizers (similar to e-cigarettes) are as high as 30 percent.15
Marijuana and Education
Marijuana use negatively impacts educational achievement.4 A recent study revealed that heavy marijuana use during the adolescent years that continued through adulthood resulted in a permanent drop in IQ by eight points. A loss of eight IQ points could drop a person of average intelligence into the lowest third of the intelligence range.2Youth with an average grade of D or below were more than four times as likely to have used marijuana in the past year as youth with an average grade of A.4 High school students who use alcohol or other drugs are up to five times more likely to drop out of school.1 Of
serious disciplinary actions in public high schools, 66.1 percent can be attributed to the distribution, possession or use of illegal drugs (school data are not disaggregated by specific drug).13
Marijuana Use and Safety
Marijuana use negatively impacts highway safety: 19 percent of teen drivers report they have driven under the influence of marijuana—only 13 percent of teen drivers report they have driven under the influence of alcohol.6According to Dr. Nora Volkow, Director of the National Institute of Drug Abuse, there have been “very, very significant increases in emergency room admissions associated with marijuana use that can’t be accounted for solely on basis of changes in prevalence rates,” rather, “It can only be explained by the fact that current marijuana has higher potency associated with much greater risk for adverse effects.”15 Emergency room visits related to marijuana have nearly doubled, surpassing alcohol-related emergency room visits from 66,000 in 2004 to 129,000 in 2011, according to the Substance Abuse and Mental Health Services Administration. Compare that to the change in emergency room visits related to alcohol, which have decreased by 22 percent from 150,988 in 2004 to 117,653 in 2011.19
Researchers at UQ’s Queensland Brain Institute and School of Population Health have found young adults who use cannabis from an early age are three times more likely to suffer from psychotic symptoms. A study of more than 3,800 21-year-olds has revealed those who use cannabis for six or more years have a greater risk of developing psychotic disorders or the isolated symptoms of psychosis, such as hallucinations and delusions. According to lead investigator John McGrath, “This is the most convincing evidence yet that the earlier you use cannabis, the more likely you are to have symptoms of a psychotic illness.”16
Marijuana and the Social Economy
According to a recent RAND study, legalization of “medical” marijuana will cause the price of marijuana to fall and its use to rise, especially among youth.7Taxes on marijuana will not cover the increased social costs associated with the increase in users. Our nation’s experiences with alcohol and tobacco show that for every dollar gained in taxes, we spend 10 on social costs.14 According to the United States Sentencing Commission, in 2008, 6,337 people were sentenced in federal court for drug crimes related to marijuana. Of these 6,337, only 1.6 percent were sentenced for simple possession of marijuana. Furthermore, according to the Bureau of Justice Statistics, only 0.4 percent of prisoners with no prior offenses are in state prisons for marijuana offenses. There does exist, however, a disproportionate rate or arrests among black marijuana users, even though statistics suggest marijuana use in the past year among black and white young people (aged 18-25) is not dissimilar.18
Marijuana Use and Medical Ethics
The FDA requires carefully conducted studies to accurately assess the benefits and risks of a potential medication. To date, there have not been enough clinical trials that show the benefits of the marijuana plant outweigh the risks in patients with the symptoms it is meant to treat; therefore, the FDA has not approved marijuana for medical use. As a result, physicians cannot prescribe “medical” marijuana. Instead, practitioners in states with laws allowing “medical” marijuana use write a letter which allows a user to obtain a card to enable the purchase of marijuana. One large barrier facing the federal government is enforcing federal laws pertaining to marijuana still being scheduled by the Drug Enforcement Administration as a Schedule I drug.
Cannabinoids (a large family of chemicals related to THC, marijuana’s main psychoactive ingredient) of interest for therapeutic reasons are THC and cannabidiol. THC stimulates appetite and reduces nausea: it may also decrease pain, inflammation, and spasticity. Cannabidiol is a non-psychoactive cannabinoid that may be useful in reducing pain and inflammation, controlling epileptic seizures, and possibly even treating psychosis and addictions. The FDA has approved the drugs Dronabinol (Marinol®) and Nabilone (Cesamet®), both used to treat nausea caused by chemotherapy and wasting disease caused by AIDS. A drug called Sativex® which contains equal parts of THC and cannabidiol is currently approved in the UK to treat spasticity caused by multiple sclerosis and is now in Phase III clinical trials in the U.S. to establish its effectiveness and safety in treating cancer pain. The FDA-approved medications lack the psychoactive ingredient which makes the user feel “high,” and are already an alternative to “medical” marijuana.8
Glossary
Age of initiation: the age at which a person uses a substance for the first time.
Cannabinoid: a class of diverse chemical compounds that act on receptors in the brain that repress neurotransmitter release, including endocannabinoids (produced in the body), phytocannabinoids (found in plants) and synthetic cannabinoids (manufactured chemically). There are two types of cannabinoid receptors in the body: type one, found in the brain (basal ganglia and limbic system, including hippocampus) and type two, found in the immune system (especially in the spleen).
Current use: use of a substance within the past 30 days.
Marijuana: dried leaves, flowers, stems and seeds from the hemp plant Cannabis sativa, which contains the psychoactive chemical delta-9-tetrahydrocannabinol (THC), as well as other related compounds; may also be concentrated in a resin called hashish or a sticky black liquid called hash oil.
Perception of risk/harm: the awareness of how little or how much risk/harm use of a substance poses to the user.
Psychoactive: pertaining to a substance having a profound or significant effect on mental processes.
Schedule I: classification for drugs, substances or chemicals with no currently accepted medical use and high potential for abuse; pose potentially severe psychological or physical dependence.
Simple possession: as pertaining to T.C.A. §39-17-418.
Social costs: the private cost plus externalities, including burden spending related to health, workforce, child and family assistance, education, mental health/developmental disabilities, public safety, and justice.
THC: primary psychoactive component of the Cannabis plant; delta-9-tetrahydrocannabinol; scheduled by the international Single Convention on Narcotic Drugs (Schedule I and IV) and by the United States Drug Enforcement Administration (Schedule I).
Author
Stephanie A. Strutner, MPH, CPSII; Executive Director, ASAP of Anderson County No conflicts of interest identified
References
1Centers for Disease Control and Prevention. 2013. Youth Risk Behavior Surveillance System. Available: http://nccd.cdc.gov/youthonline/App/Default.aspx
2 M.H. Meier, Avshalom Caspi, et al. 2012. “Persistent cannabis users show neuropsychological decline from childhood to midlife.” Proceedings of the National Academy of Sciences.
3Potency Monitoring Program Quarterly Report Number 120, Reporting Period December 16, 2012 – March 15, 2013. Mahmoud ElSohly, Director, NIDA Marijuana Project. P.7.
4Office of Applied Studies, Substance Abuse and Mental Health Services Administration (SAMHSA). SAMHSA’s National Household Survey on Drug Abuse Report—Marijuana Use among Youths. July 19, 2002. Available: http://www.samhsa.gov/oas/nhsda.htm
5Substance Abuse and Mental Health Services Administration. 2010. Office of Applied Studies. Treatment Episode Data Set (TEDS): 2009 Discharges from Substance Abuse Treatment Services, DASIS. Available:
http://wwwdasis.samhsa.gov/webt/quicklink/US10.htm
Also see Non-medical cannabis: Rite of passage or Russian roulette? 2011. Center on Addiction and Substance Abuse, Columbia University.
6Hazy Logic: Liberty Mutual Insurance/SADD Study Finds Driving Under the Influence of Marijuana a Greater Threat to Teen Drivers Than Alcohol. Available: http://www.sadd.org/press/presspdfs/Marijuana%20Teen%20Release.pdf
7Kilmer, Beau, Jonathan P. Caulkins, Rosalie Liccardo Pacula, Robert J. MacCoun and Peter H. Reuter. 2010. “Altered State? Assessing How Marijuana Legalization in California Could Influence Marijuana Consumption and Public Budgets.” Santa Monica, CA: RAND Corporation, http://www.rand.org/pubs/occasional_papers/OP315
8National Institite on Drug Abuse. 2014. “Drug Facts: Is Marijuana Medicine?” Available:
http://www.drugabuse.gov/publications/drugfacts/marijuana-medicine
9 Wagner, F.A. & Anthony, J.C. From first drug use to drug dependence; developmental periods of risk for dependence upon cannabis, cocaine, and alcohol. Neuropsychopharmacology 26, 479-488 (2002). Available:
http://www.nature.com/npp/journal/v26/n4/pdf/1395810a.pdf
10 National Institutes of Health, National Institute on Drug Abuse. 2011. Topics in Brief: Marijuana. Available: http://www.drugabuse.gov/publications/topics-in-brief/marijuana
11 The National Household Survey on Drug Abuse (NHSDA) report. August 23, 2002. Available:
http://oas.samhsa.gov/2k2/MJ&dependence/MJdependence.htm
12 Lane, J., Gerstein, D., Huang, L., & Wright, D., (1998) Risk and protective factors for adolescent drug use: Findings from the 1997 National Household Survey on Drug Abuse. [Online]. Available at www.samhsa.gov/hhsurvey/hhsurvey.html; Bray, J.W., Zarkin, G.A., Ringwalt, C., & Qi, J. (2000). “The relationship between marijuana initiation and dropping out of high school.” Health Economics, 9(1), 9–18.
13 U.S. Department of Education, National Center for Education Statistics, 2009-10 School Survey on Crime and Safety (SSOCS), 2010.
14 Hazy Logic: Liberty Mutual Insurance/SADD Study Finds Driving Under the Influence of Marijuana a Greater Threat to Teen Drivers Than Alcohol. Available: http://www.sadd.org/press/presspdfs/Marijuana%20Teen%20Release.pdf
15 Moore, Abigail Sullivan. This is Your Brain on Drugs. New York Times; October 29, 2014. Available: http://www.nytimes.com/2014/11/02/education/edlife/this-is-your-brain-on-drugs-marijuana-adults-teens.html?_r=0
16 The University of Queensland, Queensland Brain Institute and School of Population Health; February 28, 2010. Available: http://www.uq.edu.au/news/article/2010/02/early-cannabis-users-three-times-more-likely-have-psychotic-symptoms
17Substance Abuse and Mental Health Services Administration. 2010. Office of Applied Studies. Treatment Episode Data Set (TEDS): 2009 Discharges from Substance Abuse Treatment Services, DASIS. Available:
http://wwwdasis.samhsa.gov/webt/quicklink/US10.htm
18 Matthews, Dylan. The black/white marijuana arrest gap, in nine charts. The Washington Post; June 4, 2013. Available: http://www.washingtonpost.com/blogs/wonkblog/wp/2013/06/04/the-blackwhite-marijuana-arrest-gap-in-nine-charts/
19 Substance Abuse and Mental Health Services Administration. 2011. Center for Behavioral Health Statistics and Quality. Drug Abuse Warning Network (DAWN): 2004-2011. National Estimates of Drug-Related Emergency Department Visits. Available: http://www.samhsa.gov/data/sites/default/files/DAWN2k11ED/DAWN2k11ED/DAWN2k11ED.pdf
Shoveling Up the Consequences
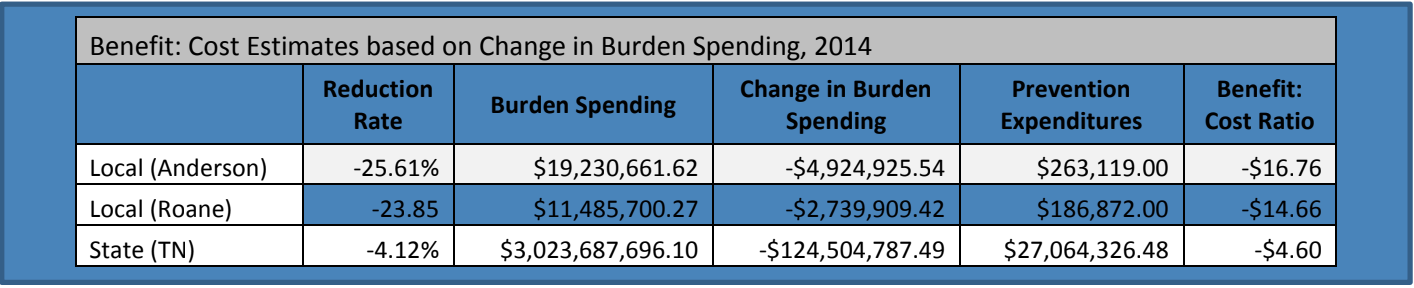
A study completed by the National Center on Addiction and Substance Abuse at Columbia University (CASA) finds, “for every dollar the federal and state governments spent on prevention and treatment, they spent $59.83 shoveling up the consequences” of our failure to prevent and treat the problem.
The largest impact on spending to “shovel up” the consequences of substance use “would be to make significant investments in prevention to help avoid the costs altogether.” 3
2ICF International. (2012). Drug free communities support program national evaluation 2011 interim findings report. Retrieved from http://www.whitehouse.gov/sites/default/files/ondcp
/grants-content/2011_dfc_interim_report_final.pdf
3The National Center on Addiction and Substance Abuse at Columbia University (CASA). (2009). Shoveling Up II: The Impact of Substance Abuse on Federal, State, and Local Budgets. National Center on Addiction and Substance Abuse at Columbia University (CASA).