Complementary and Alternative Medicine (CAM) Effectiveness for Pain Treatment
COMPLIMENTARY AND ALTERNATIVE MEDICINE (CAM)
EFFECTIVENESS FOR PAIN TREATMENT
Origins of Complementary and Alternative Medicine (CAM)
According to the Institute of Medicine of the National Academies (2005), it is difficult to pinpoint an exact date for the founding of many complementary and alternative therapies because some of them, such as acupuncture, date back hundreds or even thousands of years.
In 1998, Congress authorized the Office of Alternative Medicine into an independent center at the National Institute of Health and renamed it the National Center for Complementary and Alternative Medicine (NCCAM). NCCAM researches the effectiveness and safety of various complementary and alternative medicines and therapies as they relate to improving healthcare and services. Now called the National Center for Complementary and Integrative Health (NCCIH), this office has conducted many scientific studies designed to test the safety and efficacy of various complementary and alternative medicines and provides research-based information on complementary and alternative medicine.1
This white paper explores the history of pain treatment in Tennessee, pain pathways and effective methods of treatment, and the efficacy of CAM pain management.
Intractable Pain Treatment Law
The Intractable Pain Treatment Act was created on May 21, 2001. This legislation was enacted, in part, to remove physician fears of prescribing opioid pain relievers to patients with severe, intractable pain. Although opioid safety was mentioned in the Act, this piece of legislation gave physicians the discretion to prescribe opioid pain relievers as a first-line drug for pain. This is significant because the Act allowed physicians to prescribe opioid pain relievers instead of treatments or alternative medications that would effectively help relieve pain. According to this Act, prescribing physicians were required to either prescribe opioids or to refer the patients to a prescribing physician who will prescribe opioids to the patient.2
Developments to Supplement the Law
There were supplements added to the law in order to help combat opioid abuse. Included in the original Act, there were provisions that were intended to prevent opioids from getting into the
hands of those who would misuse opioid prescriptions. In 2002, the state of Tennessee implemented the Controlled Substance Monitoring Act, which created a statewide database, commonly called the Controlled Substance Monitoring Database (CSMD), to monitor Schedule II, III, IV, and V substance sales and distribution. The CSMD started collecting data on December 1, 2006. The Prescription Safety Act of 2012 further enhanced the capabilities of the CSMD and created stricter requirements for its use.2
In 2015, the State of Tennessee repealed the Intractable Pain Treatment Act.3
Opioid Epidemic and Pain Treatment
Prescriptions are cheaper in the short run but at the cost of addiction and overdose deaths. Before considering pain treatment, it is helpful to distinguish between types of pain.
Understanding Pain
Acute pain and chronic pain are different processes. Acute pain is mostly driven by the tissue damage (although our thoughts and our emotions affect it somewhat). In contrast, chronic pain is driven mostly by our thoughts and emotions, and tissue damage is less important.4
Figure 1: Acute and chronic pain drivers (provided by Don Teater, MD, MPH)
Four Types of Pain
Dr. Don Teater, family physician and expert contributor to the CDC Guideline for Prescribing Opioids for Chronic Pain (2016), has described four types of pain.4
• Nociceptive pain: Pain results from tissue damage causing activation of the nociceptor nerve fibers. The activation of these nerves sends a signal to the brain that causes pain.
• Neuropathic pain: This occurs when there is damage to the nerves that transmit the pain signal. The damage to the nerve causes it to activate when it should not. This results in pain that is perceived at the origin of the nerve process. A typical example of this is a herniated disc impinging on the sciatic nerve. The problem is in the lower back but the pain is felt in the foot or lateral aspect of the lower leg.
• Central sensitization: This occurs when the modulation function of the brain and central nervous system is broken and negative thoughts, memories, and emotions magnify the pain. Very mild pain may be greatly magnified causing it to become life-altering. In some situations, the pain may be entirely generated by our brain. We believe that this is the case in fibromyalgia and many cases of chronic low-back pain.5
• Opioid-withdrawal pain: People on opioids for more than a few days will usually have more pain as the opioids are reduced or stopped. This increased pain may make individuals think that their pain problem has worsened. For this reason, many people on chronic opioid therapy think that they cannot stop their medications. They have tried in the past and their pain was worse than ever. After they stop their medications for several weeks, their pain will actually improve, but the process of stopping is very difficult.6
Efficacy of Pain Medications
Different pain responds to different medications.7
• Nociceptive pain responds very well to non-steroidal anti-inflammatory drugs (NSAIDs) and acetaminophen (Tylenol). There is abundant evidence that NSAIDs and acetaminophen are more effective than opioids in nociceptive pain. The main advantage of opioids is that they are very calming which is important in severe trauma and end-of life situations.7
• Neuropathic pain responds best to many medications that are also used for seizures such as gabapentin and carbamazepine.
• Central sensitization (CS) is best treated with behavioral therapy to reduce the anxiety, depression, and automatic negative thoughts. CBT and mindfulness therapy has the most evidence of effectiveness – even more than any medication. Opioids in CS initially make people feel much better but in the long term, they make the pain worse.
• Opioid-withdrawal pain has no easy solution. Behavioral therapy to reduce catastrophizing is helpful. Simple education on what is happening also will help. 7
What is “effective” pain relief?
Fifty percent relief of pain is considered effective treatment, allowing people increased functional abilities and an improved quality of life. Number Needed to Treat (NNT) is the number of people who must be treated by a specific intervention for one person to receive a certain effect. How many people must be treated with a certain dose of a medication for one person to receive 50 percent pain relief (effective relief)? The lower the NNT, the more effective the treatment.7
The Cochrane Collaboration is highly respected globally for its scientifically rigid, independent reviews. Several Cochrane reviews have examined the treatment of postoperative pain. Postoperative pain is often studied because it is an example of acute pain where there has been tissue trauma resulting in pain. It also occurs in a controlled environment (hospital or medical office) where rigorous experimental protocols can be followed. The results of these reviews are as follows (a lower NNT means that the treatment is more effective):
• Oxycodone 15 mg
o The NNT is 4.6.
o You would have to treat 46 people for 10 to get 50 percent relief of their pain. o Thirty-six of those 46 people would not get adequate pain relief.8
• Oxycodone 10 mg + acetaminophen 650 mg
o The NNT is 2.7.
o This combination treatment is better than oxycodone alone.
o Acetaminophen adds significant benefit.8
• Naproxen 500 mg (or naproxen sodium 550 mg)
o The NNT is 2.7.
o Naproxen is not an opioid. It is an NSAID medication. Naproxen sodium is known to many as the brand name over-the-counter (OTC) medicine Aleve®.9
• Ibuprofen 200 mg + acetaminophen 500 mg
o The NNT is 1.6.
o The combination of these two OTC medicines provided the best pain relief of all.10
Current Opioid Epidemic
Although the national government does not track death rates for every drug, the National Centers for Health Statistics, at the CDC, does collect data for the most commonly used drugs. The CDC also has a searchable database called CDC Wonder. Over 72,000 Americans have died from drug overdoses in 2017, including all illicit drugs and prescription opioids. The National Centers for Health Statistics, the rate of overall drug overdose deaths have seen a 3.1 fold increase from 2002-
2017. However, the rate of opioid overdose deaths have seen a 4.1 fold increase from 2002-2017. Within the opioid overdose deaths, the prescription opioid overdose increased 1.9 fold increase from 2002-2011, but remained relatively stable since then. The fentanyl, a type of synthetic opioid, overdose rate experienced a 22 fold increase from 2002-2017. The rate of heroin overdose rates have increased 7.6 fold between 2002-2017.11
Figure 2: National overdose deaths involving opioids (provided by National Center for Health Statistics, CDC Wonder)
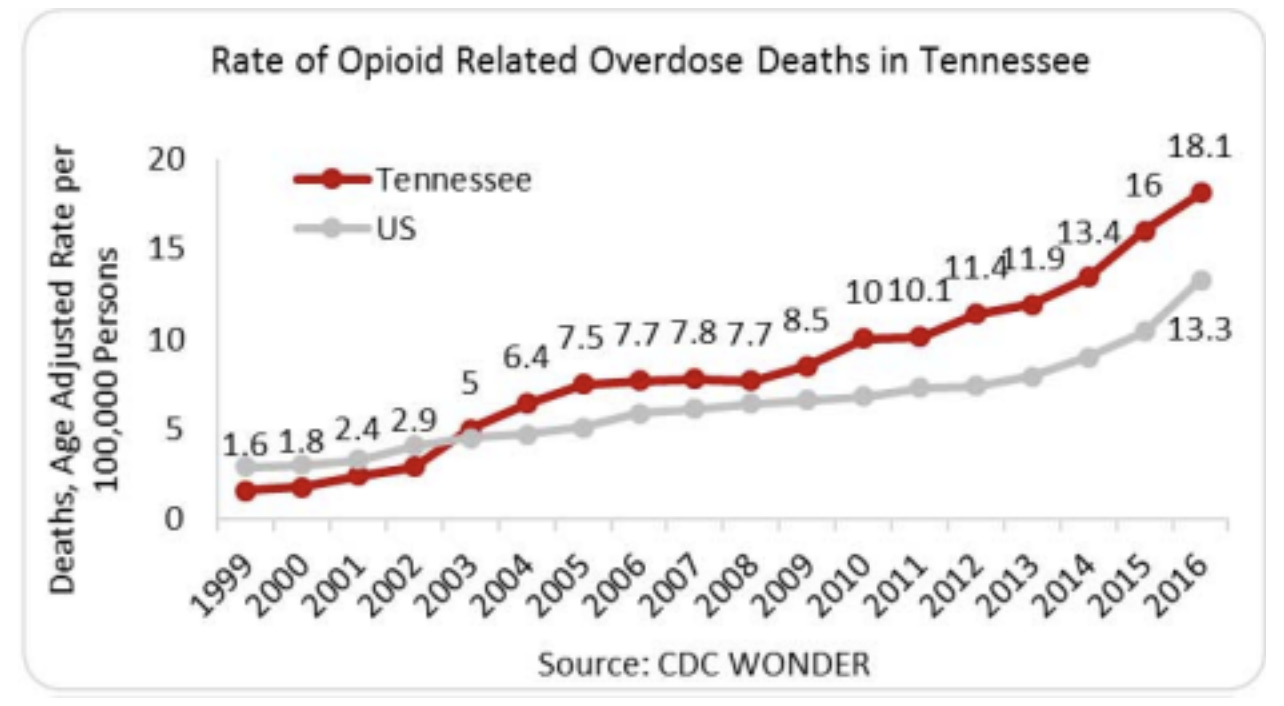
In the state of Tennessee, there is an increased rate of opioid-related overdose as compared to the national data. The overall opioid overdose deaths in 2016 the state of Tennessee saw 18.1 deaths per 100,000 persons as opposed to 13.3 deaths per 100,000 person nationally. Deaths from heroin overdoses have increased from 17 deaths in 2010 to 260 deaths in 2016. The deaths from synthetic opioids have increased from 72 deaths in 2010 to 395 deaths in 2016. The deaths from prescription opioid have increased from 516 deaths in 2010 to 739 deaths in 2016.11
Figure 3: Rate of opioid overdose deaths in Tennessee (provided by National Center for Health Statistics, CDC Wonder)
In 2015, there were 7.8 million prescriptions for opioid pain relievers in the State of Tennessee. This equates to approximately 118.3 prescriptions per 100 people. The national average for number of prescriptions written for opioid pain relievers was 70 prescriptions per 100 people.12
Efficacy of CAM Pain Management
Acupuncture
There are several studies that have been conducted on the use of acupuncture in relieving pain. One study has shown that the acupuncture meaningfully reduced the pain in palliative care patients. Patients experienced reduction in pain upon the first treatment, with subsequent reduction across all treatments.13
The Journal of Pain conducted a meta-analysis of the existing literature to determine the efficacy of acupuncture on pain relief. Thirty nine randomized controlled trials were analyzed. The results of the meta-analysis seems to confirm and strengthen the findings that acupuncture is an effective treatment for pain when compared to no acupuncture done. The effects of the acupuncture appear to be able to last up to 12 months after treatment. This meta-analysis concluded that acupuncture should be considered a reasonable option for the treatment of chronic pain.14
Chiropractic
Chiropractic care has been shown to significantly decrease lower back and neck pain. When individuals were questioned about physical functioning, pain, fatigue, sleep disturbance, social health and emotional distress, all showed significant improvement in all categories except for emotional distress.15
In addition to the decrease of pain, Chiropractic has been shown to decrease the patient’s use of opioid pain relievers. One study has shown that when veterans were receiving chiropractic care, the veterans receiving chiropractic care decreased the number of opioid prescriptions that they filled by one-third.16
It has been recommended in Canada that chiropractic clinicians use self-management supports when they treat their patients. Self-management supports have been shown to increase the outcomes of the patients. Giving the clinicians tools in order to help promote self-management supports, will tend to increase the patient outcomes.17
Physical Therapy
The American Physical Therapy Association (APTA) urges that individuals with musculoskeletal pain seek treatment with a physical therapist. APTA states that physical therapy offers good evidence-based, time-tested solutions to pain. They cite several different studies. One study, published in the Medical Journal Spine, found that when patients with neck pain received six
treatments of manual physical therapy and exercises that patients experienced pain relief. In addition to pain relief, the patients were less likely to seek additional treatment for their neck pain for up to a year. In another study, manual physical therapy and exercises were significantly more effective in decreasing mechanical neck pain and disability than a minimal intervention therapy. APTA further cites studies that show that physical therapy is more cost effective than general practitioner care.18
A smartphone app that was developed included the physician prescriptions, recommended exercise levels, and exercises. The control group was given the same information written on a piece of paper. Both groups showed decrease in pain and disability. The app group showed a significant decline in disability.19
Need for Policy Reform
Is CAM cost effective?
A systematic review examined 56 economic evaluations (39 full evaluations) of CAM covering a range of therapies applied to a variety of conditions. Of the full evaluations, 36% (14 studies) met criteria for exemplary quality and rigorous study design. These studies indicate CAM therapies may be considered cost-effective compared to usual care for various conditions:20
• acupuncture for migraine
• manual therapy for neck pain
• spa therapy for Parkinson's
• self-administered stress management for cancer patients undergoing chemotherapy • pre- and post-operative oral nutritional supplementation for lower gastrointestinal tract surgery
• biofeedback for patients with "functional" disorders (e.g., irritable bowel syndrome) • guided imagery, relaxation therapy, and potassium-rich diet for cardiac patients
Current Insurance Landscape
According to data from the 2012 National Health Interview Survey, 33% of adult and 12% of children use some form of complementary health approaches. These individuals, currently, seem to be willing to pay out of pocket for certain complementary and alternative medicines. In 2012, individuals spent $14.7 billion for out of pocket CAM practitioners, including acupuncture and chiropractors.21
Complementary and alternative medicines have been increasingly covered by insurance. In 1997 Landmark Healthcare, Inc., commissioned a national survey of HMO use of CAM. In 114 HMOs surveyed, 67% offered at least one CAM to be covered. The most common alternative therapies were chiropractic care and acupuncture. A study conducted in 1999 found that almost all health insurance plans provide some form of reimbursement or coverage for chiropractic care. Included in the study was that nearly 40% covered acupuncture and 37% covered massage therapy. Another article indicated that there was an increasing trend, between 1998 and 2000, to moderately increase the coverage of different complementary and alternative medicines and treatments (Institute of Medicine). Scientific evidence suggests that some complementary health approaches are safe and effective methods that may help people manage chronic pain. The National Center for Complementary and Integrative Health has a database of evidence-based options to use complimentary modalities to effectively and safely treat chronic pain.22
Recommendations
State-funded insurance, along with private insurance providers, should cover complimentary pain treatment modalities deemed to be effective by the National Center for Complementary and Integrative Health in an effort to reduce substance use disorder, increase the effectiveness of pain treatment, and increase access to effective care.
Glossary
Complementary and Alternative Medicine (CAM) - A group of diverse medical and health care practices and products that are not presently considered to be part of conventional medicine.
Number needed to treat (NNT) - NNT is the number of people who must be treated by a specific intervention for one person to receive a certain effect.
References
1“NCCIH Facts-at-a-Glance and Mission.” National Center for Complementary and Integrative Health, U.S. Department of Health and Human Services, 24 Sept. 2017, nccih.nih.gov/about/ataglance.
2Prevention Alliance of Tennesee, (ND), White Paper Summary on Intractable Pain Act. 3Wadhwani, Anita. “Tennessee laws to fight opioid abuse.” Tennessean, 2 Apr 2016.
4Teater, M., & Teater, D. (2017). Treating Chronic Pain: Pill-Free Approaches to Move People from Hurt to Hope. Eau Clair, WI: PESI Publishing & Media.
5Davis, B., & Vanderah, T. (2016). A new paradigm for pain? The Journal of Family Practice, 65(9), 598–605.
6Rieb, L., Norman, W. V, Martin, R., Berkowitz, J., Wood, E., McNeil, R., & Milloy, M. (2016). Withdrawal-associated injury site pain (WISP): a descriptive case series of an opioid cessation phenomenon. Pain, 157(12), 2865–2874. https://doi.org/10.1097/j.pain.0000000000000710
7Teater, D. (2014). Evidence for the efficacy of pain medications. Itasca, Illinois. Retrieved from http://media.wix.com/ugd/cb52b5_8a3726bdfc2c47fa9da81547e622cb45.pdf
8Gaskell, H., Derry, S., Moore, R., & McQuay, H. (2009). Single dose oral oxycodone and oxycodone plus paracetamol (acetaminophen) for acute postoperative pain in adults. Cochrane Database of Systematic Reviews, (3). doi:10.1002/14651858.CD002763.pub2